Sometimes, clear communication is one saved life.
In the medical field, this is no figure of speech – it’s reality. From daily rounds to life-or-death moments, communication is integral to every phase of medical work. And yet, it’s often the one that breaks first.
Busy shifts, endless handovers, details splintered over platforms – these are common challenges for medical professionals. The stakes are high, the tempo is brisk, and there’s usually little time to double-check who knows what. Balancing multiple systems not only slows it down, but it can also create mental overload, errors, and failures in coordination. That’s when things begin to fall apart.
This is exactly why real-time communication matters. It gives clarity during moments that can’t wait. It makes teams stay in sync, even across departments, floors, or buildings. And it prevents noise so the right individuals get the right information, at the right time.
This is where an application like Chanty becomes essential. It gives medical staff a single, reliable platform to message, call, share updates, assign tasks, and stay on track – without switching tools or losing time. You can see how it works in real clinical teams and explore how it fits into the fast, demanding pace of modern healthcare. It’s simple to set up, easy to use, and designed to support collaboration in hospitals, clinics, and beyond.
In the sections that follow, we’ll look at what medical communication really involves, the most common barriers teams face, and how the right tools – including Chanty – help solve them.
What is medical communication and how is it different?
Medical communication is the exchange of critical information between healthcare professionals, patients, and systems. It must be delivered clearly, under pressure, and with no room for error. So it’s not just about talking. It’s about making sure the right person hears the right message at the right time and understands it completely. In simple terms, it’s a structured and timely transfer of healthcare information that directly impacts clinical outcomes.
What sets it apart from business or everyday interactions is the level of responsibility that goes with every word. A misdirected message there does not translate into a missed deadline. It can decide a person’s health, well-being, or life.
In a medical setting, communication is usually involves multiple roles – doctors, nurses, technicians, pharmacists, support personnel – with different tools, schedules, and priorities.. Yet they must act as one.
There’s no room for vague instructions or guesswork. All messages must be clear, concise, and verifiable. They have to move seamlessly from shift to shift, department to department, and sometimes from language to language. Unlike in other workplaces, healthcare teams rarely get a second chance to clarify. Timing and accuracy here can make all the difference.
Medical communication is also layered. It’s not only about staff coordination. It includes patient education, family updates, and coordination with outside providers. Each level carries its own tone, content, and urgency, and each must be handled with care.
And finally, it’s emotional. Healthcare professionals experience stress, fear, and loss, but stay professional and calm. How they communicate must be able to carry that emotional load, not exacerbate it.
This complexity is exactly why healthcare teams need tools that work with them, not against them. Solutions like Chanty, designed specifically for healthcare, help speed up critical decisions, reduce administrative burdens, and keep teams connected in real time – all without adding to the stress. By bringing messaging, task management, and secure file sharing into one easy-to-use platform, Chanty supports clearer, faster, and safer collaboration across departments, shifts, and locations.
Effective medical communication stands apart for its precision, emotional depth, and impact. It’s not just the exchange of information – it’s the foundation of safe, coordinated, and compassionate care. And to make it work, we need to understand what still gets in the way, and how to break those barriers down.
5 Critical сomponents of medical communication every healthcare team must master
Breaking medical communication into its parts makes it clearer and easier to understand how it works. There are five components: Sender, Message, Channel, Receiver, and Feedback. Each performs a different task. They all work together to form the complete picture of how information moves in a healthcare environment.
1. Who sends the message
It all starts with the sender. This is the person who possesses the information to convey. In medicine, it can be a doctor explaining a diagnosis, a nurse explaining a change in vitals, or a technician alerting the team about a test result.
The sender carries the responsibility of being clear, accurate, and on time. If the message is not clear or complete, the entire process is already tainted.
2. What the message really carries
Message is the material – what needs to be conveyed. In health care, it might be medication orders, lab results, or a shift report. Verbal, written, visual, even nonverbal.
The point is that the message must be unambiguous to comprehend. No room for confusion, especially where decisions are being made in real time.
3. The right channel
The channel is the way in which the message is being passed. It can be face-to-face, by a call, by a note, or on a computer platform like an imbedded secure messaging program.
This step is often an afterthought, but it is crucial. The incorrect channel can delay the message and also corrupt the message. And in medicine, delaying and distorting are real dangers.
4. Who needs to hear it
The receiver is the one who receives the message. It could be another medical practitioner, the patient, or a relative. The receiver must be able to prepare and receive the information in a clear manner.
That’s why there is a need to personalize the message according to the receiver’s role and level of knowledge. One size does not fit all in this case.
5. How we know it was understood
Feedback closes the loop. It verifies that the message was received – and more importantly, interpreted. This is sometimes skipped in high-speed systems. But that’s when mistakes happen.
A simple confirmation, a re-broadcasted directive, or a prompt reply can prevent a misunderstanding from ever becoming a mistake.
What breaks medical communication?
Even when systems are in place, medical communication doesn’t always flow as it should. There are obstacles – sometimes open, sometimes hidden – that get in the way. And when they do, the dangers aren’t technical. They’re deeply human.
Let’s look at the most common ones.
Language barriers
Language differences are among the most visible and impactful obstacles in healthcare communication. When the patient and clinician don’t share a fluent language, even simple exchanges can lead to misunderstanding.
A wrong “yes” or a hesitant “no” can change the course of treatment. Critical details may be skipped, or patients might agree out of politeness rather than understanding. Language barriers can appear on either side – patient or healthcare team – and in diverse medical settings, this is a daily challenge.
Cultural barriers
Culture influences how people talk about pain, privacy, and trust in medical contexts. Some patients avoid eye contact as a sign of respect, while others prefer not to speak openly in front of family. Certain illnesses may be stigmatized, and some treatments may clash with personal beliefs.
When medical teams overlook these cultural nuances, even clear instructions may fail to connect. Cultural barriers are often invisible until they directly affect care and decision-making.
Medical jargon
Medical professionals rely on precise terminology to stay efficient and accurate. But what’s clear to staff can sound foreign to patients. Words like “hypertension,” “biopsy,” or “benign” may seem small but can cause confusion or fear.
While jargon helps streamline communication among professionals, it often widens the gap with patients – especially when emotions run high or stress interferes with comprehension.
Low health literacy
Low health literacy is another major communication barrier. Some patients struggle to interpret medical terms, even when they’re simplified. Instructions, consent forms, and prescriptions can feel overwhelming.
Patients may nod along to avoid embarrassment or skip questions to not appear uninformed. This silent misunderstanding often remains hidden until it leads to a serious mistake in care.
Disabilities
Disabilities that affect hearing, vision, cognition, or speech directly impact how communication happens. A deaf patient may miss verbal instructions, a person with dementia may not retain complex directions, and someone with a speech disorder may have difficulty expressing pain.
These aren’t rare exceptions – they’re common realities. Effective communication in healthcare requires adapting how information is shared, not just what is said.
Lack of time
Time pressure is one of the most common and underestimated causes of poor communication in healthcare. Rushed consultations, brief handovers, and overloaded schedules reduce opportunities for clarity and empathy.
When there’s no time to double-check understanding, small missteps turn into big errors. Time constraints don’t just affect efficiency – they directly threaten the quality of medical communication.
Emotional stress
Hospitals are high-stress environments for everyone – patients, families, and healthcare professionals. Fear, pain, burnout, or frustration can cloud both listening and speaking.
Under stress, communication shortens, tone changes, and patience runs thin. Even strong communication skills can falter unless systems are in place to reduce emotional strain and support meaningful connection.
Communication failures are rarely about words alone
Each of these barriers – from language and culture to stress and time – reveals how fragile human connection in healthcare can be. Medical communication breaks not because people don’t care or try, but because real-life pressures, emotions, and contexts interfere.
Recognizing these challenges is the first step toward building systems and practices that make communication clear, compassionate, and safe for everyone involved.
Tools that help overcome medical communication barriers
| Barrier | Tool & Key Feature | How It Helps | How Chanty Supports This |
| Language barriers | MediBabble – Instant medical phrase translation in multiple languages | Helps providers communicate with non-native speakers without delay | Text-based messaging helps clarify instructions; attach translated documents or notes easilyShare interpreter contact links or summaries; keep everyone on the same page |
| Jeenie – On-demand human interpreters | Real-time interpreter access for clinical use | ||
| Cultural barriers | CultureVision – On-demand cultural guidance | Offers insights into health beliefs, communication norms | Enables quick team chats to align approach before patient interaction |
| Medical jargon | Health Literacy Advisor – Flags complex language in documents | Rewrites patient-facing content in simpler terms | Use message templates and simple language for staff handovers and updatesStore simplified explanations in shared threads or files |
| UpGo – Jargon simplifier powered by AI | Converts clinical language into lay terms for patients | ||
| Low health literacy | Teach-Back Tool – Patient education with repetition and visual aids | Helps ensure understanding through interactive learning | Share visuals, infographics, or summary videos directly in chat or task threadsUpload or link short videos and files in secure, structured conversations |
| Mytonomy – Patient engagement videos | Makes complex instructions easier to digest | ||
| Disabilities | Ava – Live captions for the deaf and hard of hearing | Provides instant on-screen transcription during conversation | Share transcribed notes, voice messages, and visuals; supports both written and spoken inputAccepts any file type; allows collaboration without relying solely on spoken language |
| Proloquo2Go – Speech aid for nonverbal users | Helps patients communicate using symbols and phrases | ||
| Lack of time | TigerConnect – Real-time clinical messaging with prioritization | Enables fast, secure team updates and alerts | Set up group channels, mention colleagues, assign tasks instantly from chatEnables fast text or voice replies without switching tools |
| Vocera Edge – Hands-free voice command system | Speeds up information exchange during emergencies | ||
| Emotional stress | Well-Being Index – Emotional health check-in for medical staff | Tracks emotional fatigue and supports mental wellness | Teams can share updates async, reduce noise, and structure conversations around focusShared links, reminders, or reflections can be part of team wellness threads |
| Headspace for Work – Guided mindfulness for care teams | Supports stress relief and focus before or after demanding shifts |
Why Chanty is great for medical communications?
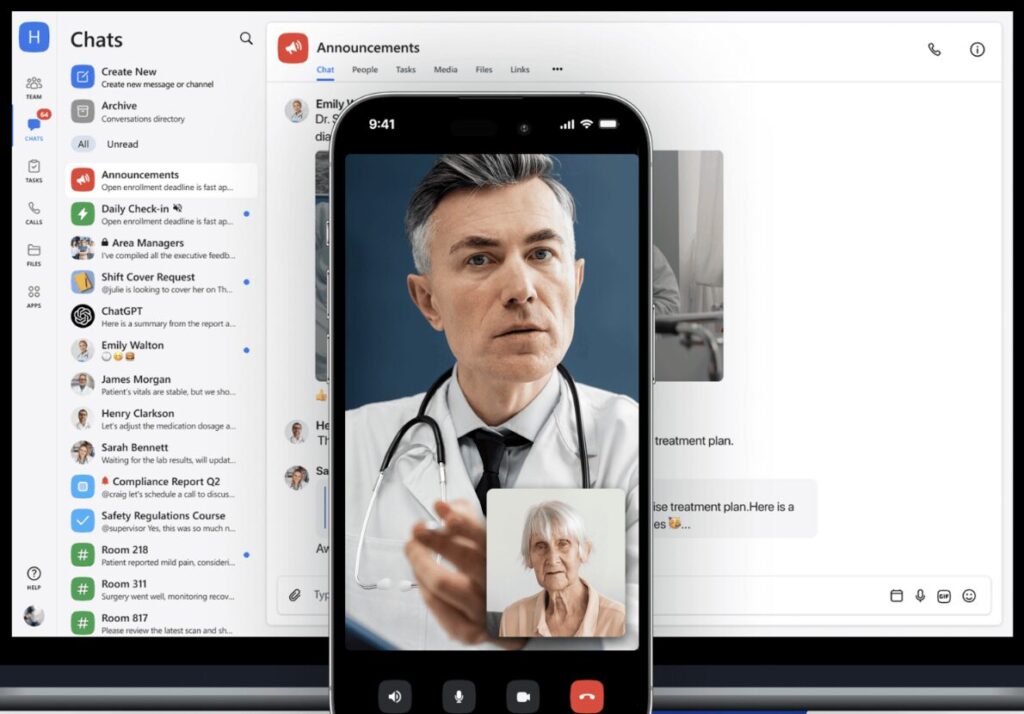
Healthcare teams have no time to fight with tools. You require something that hits the ground running, stays organized, and makes people get along, even in the middle of a crazy shift. That’s where Chanty enters.
It’s simple. Fast to set up. And powerful in ways that really count.
Turn messages into action
In Chanty, anything can be readily transformed into a task with one click. Be it a room that requires cleaning, a lab test to check up on, or a handover note from a shift, you just transform, assign, and follow through in the Kanban board.
No copying stuff over to another system. No forgetting. You stay organized without extra effort.
Talk to the right people — not everyone
With @mentions, updates go straight to the person who needs to act, not the whole group. Whether it’s a nurse on the next shift, a lab tech, or a department head, they get notified without creating unnecessary noise for others.
That clarity keeps teams focused and cuts down on delays.
Already using tools? we’ll work with you
Most healthcare teams already rely on systems such as EHRs or EMRs. Chanty presently does not support direct integration with those systems, and we’re not proud to say so.
But we move fast, too. If your team needs to integrate Chanty into your existing systems, our developers are happy to try and figure out how we can make it work together. A number of our customers made custom installs with us in days or weeks.
We believe software should adapt to your reality, not the other way around.
Strong on privacy, built for safety
Healthcare information has to stay safe. With IP Allowlisting, you control who can get into your Chanty workspace, and where. That keeps sensitive data in and unwanted users out.
It’s a quiet but vital layer of security.
Clean, quiet, focused
Some systems try to do everything. Chanty stays simple by design. Messages, tasks, files, and voice notes — all in one place, without chaos.
Need one location for patient rounds, a separate one for scheduling, and another for handovers? All done. Everything’s organized, searchable, and a breeze to keep track of — even at the end of a long shift.
Adapts to the real speed of healthcare
Healthcare workflows are non-linear. Priorities shift mid-shift. People work between sites. Things happen fast.
Chanty allows you to leave a voice message from room to room, send a document on the move, or review later when you find some time. It fits your schedule, not the other way around.
Adapts to your team size and style
Chanty is naturally modular. You can set up a small clinic on a few channels — or stretch across numerous teams in a big hospital. No further training. No ramp-up.
And when you need to adjust, it’s easy to rework your workspace within minutes.
A note on what’s still improving
We’re proud of what Chanty provides. But we also know it’s not completely perfect. Currently, there is no out-of-the-box direct integration with EHR and EMR systems. Some teams get around this using shared files and tag-based tasking, but we realize fuller integration is necessary, and we’re willing to work with you to create it.
Also, group video calls sometimes experience minor glitches, especially on older networks or slower devices. One-on-one calls run smoothly, but we’re actively refining the group call feature to improve performance.
Final thoughts
Medical communication isn’t a secondary function — it’s the heartbeat of care. It shapes decisions, builds trust, and saves lives. From the slightest message to the most urgent call, each exchange matters.
In this post, we explored what medical communication actually is. We looked at the five core things that hold it together. We named the silos that break it apart — from language barriers to time pressure. And we showed how the right tools, like Chanty, can keep teams clear, on the same page, and on the same mission.
Because the truth is, doctors already have enough to deal with. They push through fatigue, stress, and impossible schedules — all to save others. And even routine team interactions shouldn’t be another burden on their shoulders.
That’s why we built Chanty to make collaboration as simple and supportive as possible. So teams can spend less time on finding updates and more on what matters most: care, clarity, and human connection. If you’d like to schedule a free demo, we’ll walk you through how it could work for your clinic or hospital, no pressure, just possibilities.
In the end, better teamwork isn’t just about efficiency. It’s about shedding the burdens of stress, easing the chaos, and helping medical teams to have their work done without the overwhelming noise. And that, we believe, is worth building for.